Physical Medicine and Rehabilitation Division
Kuo-Hsien Tu, MD
De Quervain syndrome as BlackBerry thumb, gamer’s thumb, washerwoman’s sprain, radial styloid tenosynovitis, de Quervain disease, de Quervain’s tenosynovitis, de Quervain’s stenosing tenosynovitis, mother’s wrist, or mommy thumb), is a tenosynovitis of the sheath or tunnel that surrounds two tendons that control movement of the thumb.
Symptoms
Symptoms are pain, tenderness, and swelling over the thumb side of the wrist, and difficulty gripping.
Causes
The cause of de Quervain’s disease is not established. Evidence regarding a possible relation with occupational risk factors is debated. A systematic review of potential risk factors discussed in the literature did not find any evidence of a causal relationship with occupational factors. However, researchers in France found personal and work-related factors were associated with de Quervain’s disease in the working population; wrist bending and movements associated with the twisting or driving of screws were the most significant of the work-related factors. Proponents of the view that De Quervain syndrome is a repetitive strain injury consider postures where the thumb is held in abduction and extension to be predisposing factors. Workers who perform rapid repetitive activities involving pinching, grasping, pulling or pushing have been considered at increased risk. Specific activities that have been postulated as potential risk factors include intensive mouse/trackball use and typing, as well as some pastimes, including bowling, golf and fly-fishing, piano-playing, and sewing and knitting.
Women are affected more often than men. The syndrome commonly occurs during and after pregnancy. Contributory factors may include hormonal changes, fluid retention and—more debatably—lifting.
Pathophysiology
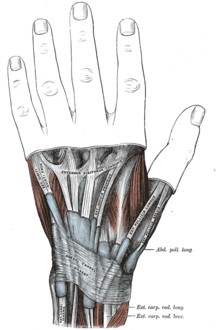
The mucous sheaths of the tendons on the back of the wrist.
The two tendons concerned are the tendons of the extensor pollicis brevis and abductor pollicis longus muscles. These two muscles, which run side by side, have almost the same function: the movement of the thumb away from the hand in the plane of the hand—so called radial abduction (as opposed to movement of the thumb away from the hand, out of the plane of the hand, or palmar abduction). The tendons run, as do all of the tendons passing the wrist, in synovial sheaths, which contain them and allow them to exercise their function whatever the position of the wrist. Evaluation of histological specimens shows a thickening and myxoid degeneration consistent with a chronic degenerative process. The pathology is identical in de Quervain seen in new mothers.
Diagnosis
Finkelstein’s test is used to diagnose de Quervain syndrome in people who have wrist pain. To perform the test, the examining physician grasps the thumb and the hand is ulnar deviated sharply, as shown in the image. If sharp pain occurs along the distal radius (top of forearm, about an inch below the wrist; see image), de Quervain’s syndrome is likely.
Treatment
Most tendinoses are self-limiting and the same is likely to be true of de Quervain’s although further study is needed.Palliative treatments include a splint that immobilized the wrist and the thumb to the interphalangeal joint and anti-inflammatory medication or acetaminophen. Systematic review and meta-analysis do not support the use of splinting over steroid injections.
Surgery (in which the sheath of the first dorsal compartment is opened longitudinally) is documented to provide relief in most patients. The most important risk is to the radial sensory nerve.
Some physical and occupational therapists suggest alternative lifting mechanics based on the debatable theory that the condition is due to repetitive use of the thumbs during lifting such as seen in new mothers picking up their child. Physical/Occupational therapy can suggest activities to avoid based on the theory that certain activities might exacerbate one’s condition, as well as instruct on strengthening exercises based on the theory that this will contribute to better form and use of other muscle groups, which might limit irritation of the tendons. This approach may risk reinforcing catastrophic thinking (pain catastrophizing) and kinesiophobia.
Some physical and occupational therapists use other treatments based on the rationale that they reduce inflammation and pain and promote healing: UST, SWD, or other deep heat treatments, as well as TENS, dry needling, or infrared light therapy, and cold laser treatments. However, the pathology of the condition is not inflammatory changes to the synovial sheath and inflammation is secondary to the condition from friction. Teaching patients to reduce their secondary inflammation does not treat the underlying condition but may reduce their pain.
