Kuo-Hsien Tu
Introduction
Plantar fasciitis is inflammation of plantar fascia of the foot. It is a relative common painful foot condition. About one in 10 people will develop plantar heel pain during their lifetime.
Anatomy
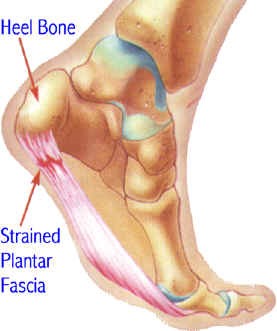
The plantar fascia arises from the medial tuberosity of the heel bone (calcaneus) and attaches into the bases of toes. It is important in keeping the foot arch and winding up all the toes during stance phase of walking cycle. It is also known as ‘windlass mechanism’.
Cause
Plantar fasciitis is associated with tight heel cord, recent gain of weight, trauma, running activities and after wearing a new pair of shoes.
Symptoms
The typical symptom is pain under the plantar heel. The pain usually gets worse on initial weight bearing in the morning and after sitting for a prolonged period of time. The pain often improves with further walking but then returns after prolonged standing or walking.
Diagnosis
Plantar fasciitis is most often diagnosed clinically by the typical symptoms and tenderness at the medial tuberosity of the heel bone (calcaneus). There are other causes of plantar heel pain such as nerve entrapments, stress fractures, fat pad atrophy, tarsal tunnel syndrome and rheumatologic conditions including ankylosing spondylitis.
People often confuse the terms heel spur and plantar fasciitis. Heel spur is a “bony outgrowth” from posterior tuberosityof the calcaneus. Half of the patients with plantar fasciitis will have a heel spur on x-ray but 15% of normal population will also have a spur. Therefore, presence of heel spur does not mean the occurrence of symptoms or plantar fasciitis. X-ray may be taken to rule out other causes of heel pain such as stress fracture or tumour.
Non-surgical treatment
Conservative treatment is the mainstay for plantar fasciitis. The initial treatment includes rest, insole, night splint, anti-inflammatory drugs, stretching exercise and physiotherapy. Local injection of steroid can provide pain relief, but repeated injections will have higher risk of fat pad atrophy and fascia rupture. If symptoms persist for more than 6 months, shock wave therapy should be considered..
general, more than 90% of patient will improve with conservative treatment by 6 months.
Surgical treatment
For patients whose symptoms persist for more than 6 to 9 months despite conservative treatment, surgery might be considered. Part of the plantar fascia is released from its origin. Unfortunately, the outcome of surgery for plantar fasciitis is not so ‘predictable’. Surgical risks include persistent pain, flat foot deformity, nerve injury and infection.